As the epidemic enters an uncertain winter, millions of Americans have little options if they get sick because to the absence of specific Covid-19 medications for those with weakened immune systems.
Monoclonal antibodies were once hailed as game-changers for Covid patients thought to be at risk of becoming gravely ill; one was used to treat then-President Donald Trump in 2020. However, they are now mainly useless against current Covid variations. Antiviral medications that are simpler to administer, like Paxlovid, have essentially replaced them but aren’t always safe for immune-compromised individuals due of drug interactions.
However, the federal funding that fueled the discovery of new drugs in the early stages of the pandemic has run out, and Congress have rejected the Biden administration’s requests for more. Without such, drug companies have little motivation to develop novel antibodies that might be more efficient.
Without a government initiative like Operation Warp Speed to create second-generation vaccines and medications, at-risk patients run the risk of developing severe cases of Covid and overrunning hospitals at a time when the American healthcare system is already under pressure from an influx of patients suffering from a variety of respiratory illnesses, such as flu and RSV.
Professor of public health at George Washington University and former Baltimore health commissioner Leana Wen remarked, “Just because we have left the emergency phase of the pandemic does not mean that Covid is finished or that it no longer offers a hazard.” “Millions of Americans are at risk for developing serious illnesses.”
In 2022, the FDA revoked the approvals of four antibody therapies because Omicron and its numerous subvariants rendered them ineffective. Adult and paediatric patients with mild-to-moderate Covid who were thought to be at risk of developing severe disease and needing hospitalisation received the therapies.
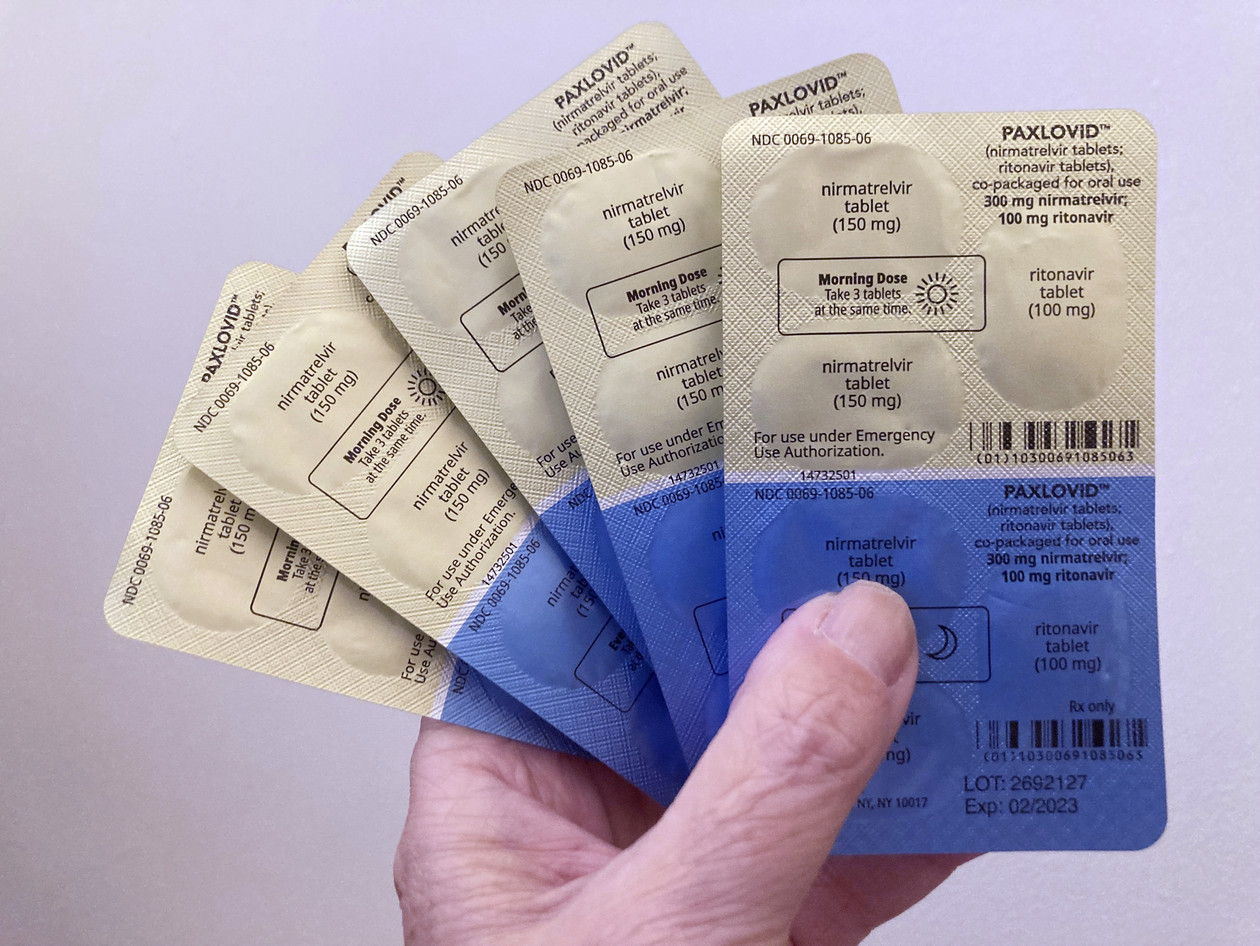
Antiviral medications are widely available and still a viable option for certain people with compromised immune systems, but not everyone will benefit from them because Pfizer’s Paxlovid interacts with a number of commonly given medications.
Monoclonal antibodies are lab-made molecules intended to prevent a virus from entering human cells. They have been produced by businesses including Regeneron, Eli Lilly, and Vir. However, in order to kill the virus, they must attach to the spike protein, and the coronavirus’s numerous modifications since its debut in 2019 have gradually rendered the available medications ineffectual.
Given how quickly some Covid variations have appeared before quickly disappearing, Arturo Casadevall of the Johns Hopkins Bloomberg School of Public Health stated, “It’s a little dangerous to produce this.”
There are fewer funds available to distribute among new Covid needs since a sizable budget measure that lawmakers passed before Christmas omitted the administration’s $9 billion request for additional funding to combat the pandemic.
A department spokesperson told AWN that HHS “does not have the resources it needs to fund the development of new treatments due to congressional inaction and a lack of funding, and we could find ourselves with a very limited medicine cabinet at a time when we need more tools to combat Covid-19.” The spokesperson also said that HHS is working with providers and other organisations “to ensure that Americans are able to take advantage of all available treatment options.”
Oral antiviral regimens like Paxlovid, which was introduced a year ago and represented a turning point in controlling the virus for most Americans, have been vigorously promoted by the Biden administration.
Immunocompromised people may not establish adequate immune responses to vaccinations, making therapy alternatives like antibody treatments a crucial tool for them. Immunocompromised people are either born with immune-suppressing disorders or develop them following organ transplants or by taking certain pharmaceuticals.
The lack of effective monoclonal antibody treatments, as well as the decreased efficacy of a prophylactic antibody, Evusheld, were both mentioned in a CDC alert sent to clinicians and public health professionals on December 20. The alert also mentioned the availability of antiviral options, though their uptake has been mediocre thus far. In order to potentially manage Paxlovid drug interactions, such as brief interruptions or dose reductions, the agency advised healthcare professionals to refer to the Covid treatment recommendations published by the National Institutes of Health.
Another therapy option for those with impaired immune systems is the intravenous antiviral remdesivir, although it necessitates three days of infusions in either a hospital or outpatient environment. HHS is asking states to assist their health departments and systems in opening infusion clinics to increase access to remdesivir, particularly for outpatients, and is collaborating with the manufacturer Gilead to expand the types of healthcare professionals who are qualified to purchase the medication.
For those with compromised immune systems who get the virus, Covid convalescent plasma is still an option, although Casadevall noted that its distribution is dispersed across the nation. It can adapt to different strains and is less likely to be overcome by any one variant, but the treatment is challenging to deliver and necessitates blood-typing for the recipient.
Even still, according to Casadevall, the primary problem is education because its application has changed since the pandemic’s early stages, when remedies were few in number. According to him, some hospital systems, like Hopkins, use plasma on a regular basis, but some doctors are unaware that it is still an option.
For patients who are immunocompromised, the FDA has approved the use of convalescent plasma with high Covid antibody levels. However, Janet Handal, president of the Transplant Recipients and Immunocompromised Patient Advocacy Group, claims that because NIH has taken a neutral stance on the medication in that demographic, some hospitals are reluctant to provide it.